Comparing activation methods to yield clinical-scale expansion of gamma delta T cells
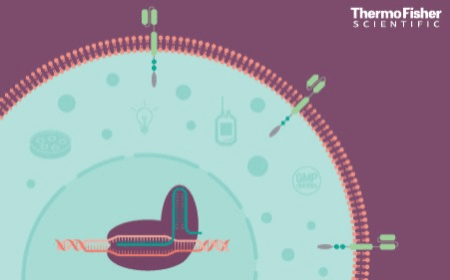
Gamma delta T cells have the inherent ability to infiltrate solid tumors and directly recognize and kill transformed cells independently of HLA-antigen presentation. Moreover, gamma delta T cells do not cause graft-versus-host disease and provide a promising platform for the development of T cell therapies targeting solid tumors. However, due to the low prevalence of gamma delta T cells in peripheral blood, it remains a challenge to generate enough gamma delta T cells to produce a clinical dose.
In this presentation, data from the use of two distinct methods to generate billions of gamma delta T cells from peripheral blood mononuclear cells (PBMCs) is compared. The first method uses zoledronic acid as the activating agent to induce the expansion of more than 1 x 10^9 Vd2+ T cells within 14 days, starting from cryopreserved PBMCs. In the second approach, either aß T cells are specifically depleted from PBMCs or gamma delta T cells are isolated via negative selection before anti-CD3 and anti-CD28 co-stimulation, generating billions of gamma delta T cells–including both Vd1+ and Vd2+ T cell subsets. The expanded gamma delta T cells exhibit innate cytotoxicity towards the K562 cell line and produce cytokines including IFN-Gamma and TNF-a. Collectively, these data indicate that both methods may be utilized to generate enough gamma delta T cells to support clinical applications.
- Learn about two methods to generate billions of gamma delta T cells from PBMCs to support clinical applications
- Find out how an anti-CD3/anti-CD28 activation method supports high lentivirus transduction of gamma delta T cells
- See data surrounding the production of Vdelta1+ and Vdelta2+ T cell subsets from PBMCs using multiple methods
You might also like
Closed and automated CAR-T production: a fast, simple workflow for high-dose, high-quality cells
End-to-end automated manufacturing of low-seed CAR-T cells
Clinical-scale non-viral gene edited CAR-NK cells for cell therapy